Starting IVs is one of the most exciting skills new nurses learn, and it can also be one of the most difficult nursing techniques to master. While threading a plastic catheter into a vein may seem straightforward when reading about it in a book, in practice, many things can go wrong or make the process more difficult. You may hear many nurses talk about “blowing a vein” when they were not successful in an IV start.
What Does It Mean to Blow a Vein?
Blowing a vein means merely that blood has leaked out of the vein into the surrounding tissue, rendering the vein unusable for IV access or blood withdrawal. The insertion site appears bruised or has developed a hematoma, and you will not be able to flush the line with saline.
What is a Blown Vein
A blown vein is a ruptured vein. This most often occurs when the wall of a vein is pierced by an IV needle. It occurs when IV insertion fails due to improper technique, frail veins, or if a patient moves. This results in blood leaking from the vein and the need to attempt an IV on a new location.
Some people also call a blown vein as:
- Blown out vein
- Blown vein IV
- Vein blown
- IV blown vein
- Blown out IV
- IV Blown
- Missed stick
- Blow out vein
- Punctured vein
The way to avoid blown veins is to improve the IV insertion technique.
Causes of a Blown Vein
Why does this happen? To understand why veins are blown you first must understand the anatomy of the vein.
Vein Anatomy
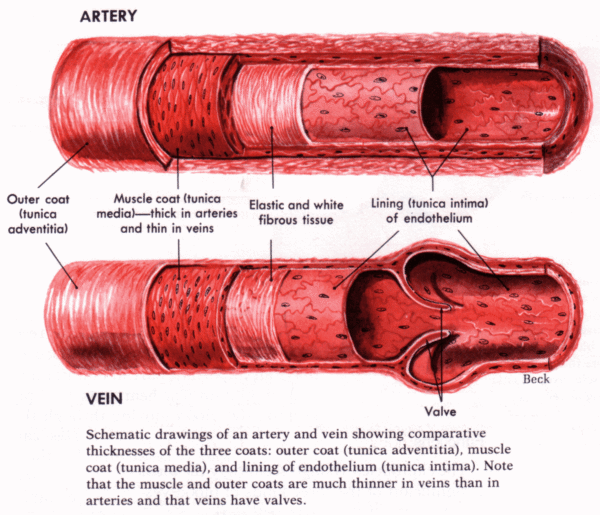
The Vein is composed of 4 separate layers: The outer layer (tunica adventitia), a muscle layer (tunica media), a thin elastic and fibrous layer, and finally the inner layer (tunica intima). When starting an IV you must pass the needle through the four layers until just the tip of the needle is in the center of the vein, then you thread a thin plastic catheter into the vein. Once you hit the tunica intima or innermost layer of the vein, you will see what is called “flashback” when the blood enters the flash chamber of your needle. Seeing a flashback does not necessarily mean you are in the vein, so when you observe a flashback, you must advance the needle about 1 mm before advancing the catheter into the vein.
Reasons for a Blown Vein
So what causes a vein to blow? Why do veins blow?
Going Through the Vein
A vein can blow for several reasons. The most common cause is that you have gone through the vein, puncturing the opposite side of the vein causing blood to leak out and creating a hematoma, often collapsing the vein and rendering it useless.
Rolling Veins
Another reason that you may blow a vein is that you have punctured to vein slightly, but it has “rolled away,” and the needle was not fully in the vein. You may have heard nurses talking about “rolling veins.” These are veins that have a slightly thicker layer of muscle and elastic tissue. When this happens, the vein can withstand the needle, rolling away and bouncing off the tip. Sometimes, however, you may puncture the tunica intima without being entirely in the vein before the vein rolls away, causing a leak and allowing blood to leak into the surrounding tissue.
Fragile Veins
Finally, some patients, especially elderly patients, have very fragile veins. If the blood is sitting in these veins at a higher pressure, they may split open when punctured by a needle. When the vein splits open like this, they usually collapse, create a large hematoma very quickly, and making the vein unusable.
What to Do if you Blow a Vein
You are starting an IV, and everything is going well when suddenly a hematoma is forming, and you realize that you have blown the vein. So what happens when you blow a vein and what should you do?
What happens when you blow a vein?
The first step is to determine if you have in fact blown the vein. Sometimes a small hematoma may form, but the catheter is sitting securely in the vein. This often happens with fragile veins, where some blood spills out upon puncturing the vein but then stops once the IV is in place. If you can advance the catheter and can flush the IV with saline easily, and there is no swelling or blanching of the surrounding tissue, this may be what has happened, and you should be able to use the IV. Be sure to monitor it closely for the first hour to ensure that no IV fluid is leaking out.
If it looks like the vein is blown and is in fact not useable, then you should remove the IV and apply plenty of pressure to the site to minimize the amount of blood that leaks out. If the hematoma is quite large or is distressing to the patient, you may apply a cold compress to the site to minimize swelling.
By and large, however, blown veins are not serious and will merely cause minor discomfort and bruising. Reassure the patient that this is not serious and warn them not to be alarmed if they do develop a bruise.
How to Avoid Blowing a Vein
While IVs can be difficult, particularly for new nurses, there are several things you can do to prevent complications such as blowing a vein. Let’s examine some IV insertion tips to help you become a great stick.
Vein Selection
When preparing to start an IV, begin by choosing the best vein possible. The ideal site for an IV is the back of the forearm. This site minimizes complications and causes the least amount of discomfort. Some people, however, do not have useable veins on their forearms due to scarring, a thick layer of subcutaneous tissue, or if their veins are very deep and not visible.
When choosing a vein, try to pick one that is straight, feels bouncy like a balloon, and is in the most convenient location, avoiding the back of the hand or the bend of the arm or wrist.
Many nurses rely on a vein finder light to help them find the best vein to use.
Optimize Vein Size
When preparing to start IVs, be sure to optimize the condition and size of the vein. If veins are small or don’t feel bouncy, try these techniques to make the veins larger and easier to see. If the vein you use is larger in size, you are less likely to go through them, causing the vein to blow.
First, try applying heat such as wrapping the arm in a warm blanket. This heat causes vein distention, making the veins larger.
Be sure to start the IV with the arm below the level of the heart. This again causes the vein to dilate further making the vein larger and less likely to blow.
If available, try using venous visual aids. These portable lights can help you identify the best vein to use, even if it is too deep to feel.
Anchor the Vein
When starting an IV, make sure you properly anchor the vein to stop it from moving around. To do this, you must apply counter pressure to the site. First, grip the skin below your planned insertion site and pull down slightly, in the opposite direction you plan on inserting the needle. This stops a ‘rolling vein’ from moving around, allowing you to successfully puncture the vein and insert the catheter.
Size of Needle
We used the think that if you can, insert the largest IV possible. Times have changed, however, and now we know that using the smallest gauge needle in the largest vein reduces the amount of discomfort from the IV and reduces any damage to the vein from caustic solutions.
Always chose the smallest gauge needle required for the task you need to complete, especially if you are inserting an IV in an older adult. As larger needles create a bigger hole, less leaking of blood should occur with a smaller needle.
Reduce the Pressure
Finally, when dealing with fragile veins the tightness of the tourniquet may increase the pressure inside the vein, causing the vein to blow as soon as the needle touches the vein. When this happens, one solution is to use a manual blood pressure cuff as the tourniquet as it gives you more control over the pressure in the vein.
When using a blood pressure cuff, the general rule of thumb is to maintain the pressure at the same level as the patient’s diastolic blood pressure. This ensures vein distention without creating excessive pressure.
If you are unsure of the patient’s blood pressure, there is another method. Often fragile veins feel hard and ‘ropey.’ Try pumping up the blood pressure cuff then releasing the valve very slowly while feeling the vein. Stop releasing pressure when the vein stops feeling hard and ropey and starts to feel soft and bouncy, like a balloon. This is the point when the vein is distended, but the pressure is not enough to blow the vein.
Alternatively, with patients who have fragile veins that are still quite large without a tourniquet, consider starting the IV without one. Also, you can apply the tourniquet to find the vein, then right before you start the IV release the tourniquet using the residual pressure for vein distention.
Starting IV is a difficult skill to master, and unfortunately, complications happen, including blowing a vein. While it is not harmful to the patient, it can be frustrating and distressing to have to attempt an IV more than one time. By following these techniques, you can avoid blowing the vein and be more successful in your IV attempts.
Try a Vein Finder Light
Vein finger lights help to illuminate the vein and make it easier to see what is going on under the skin. If you’ve never used a vein finder light, check out our article where we outline the best vein finder lights and how they work.
Reader Tips on Starting an IV if you have blown a vein
“Once you see a flash, stop.” from Tiarra
“Try again in a different location without a tourniquet.” from Olivia Mebane BSN, RN
“Sometimes if I get that “flash of blood” but can’t thread the catheter, I attach a syringe with normal saline while flushing gently and threading at the same time.
Once and only once, I blew a vein and the ER doctor said, “you’re in just thread it and flush it.” I did that and somehow pushed thru the blown vein. That IV worked the entire stay in the ER until the patient was discharged. No infiltration whatsoever. I haven’t been able to do it since though.” from Carolina “CC” Carmona BSN, CPN
Want to Upgrade Your IV Skills?
Tired of blowing veins, hurting your patients, and calling in other nurses for a successful stick?
Get the skills you need for a >90% successful stick rate on the 1st attempt!
What is the difference between collapsed veins vs blown veins?
A collapsed vein is a vein where the vessel has collapsed a the blood no longer flows. This most often occurs because the extremities are cold. A blown vein occurs when the wall of the vein has been punctured and blood escapes from the vein to create a hematoma. A collapsed vein can usually be recovered by using techniques such as arm dangling or a warm compressed. A blown vein cannot be recovered for an IV insertion. It must first heal.
See also:
- 5 Reasons Why IV Poles are a Huge Pain for Nurses
- How to Titrate a Cardizem Drip
- IV Insertion Tips for New and Experienced Nurses
- The Best Vein Finder Lights
- What Is A Phlebotomist: Certification, Salary, and Job Outlook





This was helpful to me, the patient. I’ve had two veins blown this week by two different nurses. They were very competent, but at the age of 65, my veins don’t cooperate. Thank you
Thank you! I recently had a ‘blown vein’ when a nurse was trying to get me ready for surgery. I didn’t really understand what it involved and the term sounds kind of frightening.
This clear and understandable explanation is perfect!
I appreciate it.
Great article! As a NICU nurse, we don’t have much room for error. My tip would be to keep the angle of needle as low as you can to the skin. You can always move it deeper. Keep the skin taut, I hate trying to stick the needle in and the skin is moving. Oh, and start distally you can always move up past where you have blown the vein, if you must.
I never started an IV in nursing school. I wasn’t even taught. When I finally went to try on a patient, she looked at me and said, “I hope you are better than the last person.” I thought, “Me too!”
Proper venipuncture is a skill that develops from knowledge and experience….well explained article…continue the good job
Thank you for sharing such a wonderful insight into a skill that is often fraught with pain and discomfort for the patients and nerves and frustration for the nurse. Your explaination was simple and amazing, thank you.