This article will examine the breastfeeding vs formula debate and share why fed is best.
The breastfeeding vs formula debate isn’t a new one. The debate of the quality and value of infant formula have been around since it’s invention by chemist Justus von Liebig in 1865. However, the majority of the population of new mothers have been well educated on the benefits of breastfeeding. When a child is born the parents make a decision on how to feed their child: formula, breast milk, or some combination of the two.
When a Nurse Can’t Nurse Her Child
As of the writing of this post, I’m the mother of two wonderful children. One curious, strong, and smart 9-year-old boy. And one fresh newborn baby girl. I have tried to breastfeed them both. I have failed both times. My body simply doesn’t produce breast milk. I’ve had difficulty in getting medical intervention or assessment to figure out why, but I’ve had a pituitary tumor and a weird endocrine system, which are the most likely suspects.
Breastfeeding My Child Almost Killed Him
When I had my first baby boy I was well educated on the benefits of breastfeeding. I had graduated nursing school the year before and was committed to giving my child all the immune-boosting benefits of breastfeeding. We had some difficulty with the process of latching, but he seemed to nurse. While still in the hospital, we requested the assistance of a lactation consultant who fondled my breast and provided feedback on how often and how long he should be feeding. However, I was never told of any warning signs to look for that might indicate he wasn’t getting what he should.
While still in the hospital his bilirubin levels were elevated, but they sent us home with a follow up scheduled at the pediatrician just a few days later. I continued to try to exclusively breastfeed when I was discharged from the hospital. Our baby boy was so difficult for those first few days. He cried constantly unless he was being held or nursed. And in hindsight, he had far fewer diapers than we should have anticipated and our little pumpkin was as orange as a pumpkin. But to be honest, we weren’t told to count them or to pay attention to their weight. We also were at states of near exhaustion from our constantly screaming baby and probably couldn’t have done a good job with it if we had known too.
Hyperbilirubinemia from Breastfeeding

When we visited the pediatrician, they tested his bilirubin. The politely informed us that they’d be admitting our newborn to the PICU for dehydration and hyperbilirubinemia, which is also referred to as breastfeeding failure jaundice.
Breastfeeding Failure
I was a breastfeeding failure.
For 3 days we stayed by his bedside as he sat under the bili lights with his little paper sunglasses. We started formula feeding immediately. I felt like I had failed as a mother and as a woman.
I did continue to try and pump in an effort to breastfeed my child. I’d sit in the side of the room, on the toilet (not using it, but because it was the only seat available), with the privacy curtain pulled. An entire hour of pumping would yield about 10ml of breast milk. 10ml of watery, pitiful breast milk. There is no way I could sustain my child on this.
Failure to Thrive in Breastfeeding
We were fortunate. Our issues with breastfeeding were captured early enough that our beautiful baby boy didn’t suffer any long term injuries. Some mothers aren’t so lucky. Their children can go for months of their inadequate breastmilk to be later diagnosed with failure to thrive.
Accepting that My Child Would be Formula Fed

At a post-op visit to my OBGYN, I broke down into tears because I felt I had failed as a parent. I couldn’t breastfeed my beautiful baby boy. What kind of mother was I?
I was already dealing with other emotional issues. My mother died when I was 5 months pregnant with my son. I was a new nurse in a new marriage. There was a lot on my plate and my risk for postpartum depression was through the roof.
Sensing I needed confirmation that I wasn’t going to destroy my son’s chances at a fulfilling life by formula feeding, my OBGYN said to me:
I’m the last of 6 children. My mother breastfed all my siblings, but by the time I was born, my mom was tired. So I was formula fed.
I think I turned out ok.
I think he did too.
That day I decided that if my OBGYN was formula fed then surely I wasn’t doing my child a disservice by formula feeding them. His story helped me feel like my child could still grow up to be anything they wanted regardless of how they were fed as an infant.
Attempting to Breastfeed a Second Child
After a nearly 10 year gap, my husband and I decided to have a second child. Once again, I tried desperately to breastfeed.
I was literally like a dairy cow. If I wasn’t feeding, burping, changing, or holding her, I was pumping. The time I could be up and productive was completely devoting to producing a pitiful amount of breast milk. I was much more stationary that I needed to be. I was also incredibly emotional from the stress of attempting to produce breast milk, which made me get upset and cry over almost everything. I was spending easily 4-6 hours every day on this task with almost no results. It was not healthy for me or my baby.

After 3 weeks of trying to allow my baby to feed naturally, pumping, and still only producing a maximum of 1.5 ounces for a day’s worth of effort, we made the decision to move to formula. Part of this decision was because of the strain it was putting on me emotionally as well as the impact it was making to my family dynamics.
The difference between the first child and the second child was being informed that fed is best.
I had several caring labor and delivery nurses and even a lactation consultant coach me through my attempt at breastfeeding, but they made it clear that the best interest of my child was ensuring that she was fed and I was in a healthy emotional state.
I still battled immensely with the guilt of not being able to breastfeed my beautiful baby girl, but it helped me come to terms with the right choice for our family a little sooner.
Postpartum Depression and Breastfeeding
I was a nervous wreck. My body’s inability to produce breast milk caused me to question everything. Was it my weight? Was it what I was eating? Was there something wrong with my endocrine system? What on earth could be causing my inability to produce breast milk?
I wept about it. I mourned the loss of breastfeeding my child. I felt like a terrible mother. I was on a rollercoaster with one destination: postpartum depression.
I’m not alone in this breastfeeding and depression journey.
According to Seleni.org, “A recent study published in the Maternal and Child Health Journal suggests that women with unmet expectations about breastfeeding may be at higher risk for postpartum depression (PPD).” The article goes on to highlight the association of desire to breastfeed and the ability to breastfeed:
Although researchers found that the risk of PPD was highest among the women who did not breastfeed, the increase was affected by whether the women had planned to breastfeed. Four weeks after giving birth, the women who were not breastfeeding despite wanting to during pregnancy had a fourfold increase in PPD risk compared with breastfeeding women.
It should be my biological right to breastfeed my children. The existence of the entire human race has relied upon a mother’s ability to breastfeed children. But somehow my body is broken and I simply don’t.
The Breastfeeding Vs Formula Debate
To put it simply, the breastfeeding vs formula debate shouldn’t really even be a thing. You’d be hard pressed to find any credible healthcare professional that would tell you that formula is a better source of nutrition for your baby. Breastmilk is nutritionally complete and truly is the best source of nutrients. According to Review of Infant Feeding: Key Features of Breast Milk and Infant Formula,” Formula is Infant formula attempts to mimic the nutritional composition of breast milk as closely as possible and is based on cow’s milk or soy milk.” The article goes on to conclude Breast milk is the best nutrition for infant growth and development and is also rich in antibodies that provide the first source of adaptive immunity in a newborn’s intestinal tract.”
The research makes it incredibly clear that breastmilk has nutritional and antibody benefits that can’t be debated.
In a world where every mother made breast milk without issue, mothers had sufficient paternal leave to care for their infants, babies were born on time and had no latching issues, and everything lined up perfectly: breast would always be best.
Debate over.
But this isn’t a perfect world.
Improving Breast Milk Production

For many mothers, a healthy breastmilk supply can be obtained, but it will take extra effort. Assuming your supply is in question, you will likely be pumping. Lactation consultants stress that the baby is almost always the best way to remove milk from the breast. Their latch and suck are more powerful and appropriate. If you produce milk, but cannot ensure your child is getting an adequate amount, you’ll likely be doing at least some pumping. The tips below will be specifically related to how to increase milk supply when pumping.
I’ve searched the web and read countless articles on how to increase milk production. I’ll save you some time and share the key things a mother can do to increase breast milk supply:
- Increase the rate of pumping. Pump every 2-3 hours for at least 20 minutes
- Use a high-quality breast pump to get the best results.
- The Medella Pump In Style is a fantastic pump. I do recommend spending $60 to get the Freemie Hands Free Concealable Collection Cups.
- Don’t skip pumping at night. Prolactin levels are highest at night!
- Eat adequate calories and stay well hydrated.
- Consider using herbal galactagogues to increase supply. The 3 most commonly used supplements to increase milk supply are Fenugreek, Blessed Thistle, and Goat’s Rue.
- Work with your medical provider to test your prolactin levels. If they are low you may be a candidate for pharmacological interventions such as Reglan.
- POTENT LACTATION SUPPORT: Harness the power of Goat's Rue, a powerful galactagogue renowned for its ability to significantly boost breast milk production and increase breast milk supply in lactating mothers.
- GENTLE ALTERNATIVE FOR SENSITIVE MOMS: For nursing or pumping moms who are sensitive to traditional lactation blends and milk supply supplements, Goat's Rue offers a fenugreek-free solution, ensuring effective supply support without discomfort.
- PROMOTES MAMMARY TISSUE DEVELOPMENT: Unlock the potential of Goat's Rue to foster mammary tissue growth, essential for lactation and milk production, providing the foundation for a successful breast milk supply boost and breastfeeding journey.
When Breast is Best
Breast milk is the best source of nutrition for infants when the mother can produce and provide breast milk for a child. It contains the perfect balance of nutrients essential for the infant’s growth and development. These nutrients include proteins, fats, carbohydrates, vitamins, minerals, enzymes, and antibodies that are crucial for building a strong immune system. Breast milk is also easily digestible for babies and is tailored to meet the evolving nutritional needs of the child as they grow. Additionally, breastfeeding fosters a unique bond between the mother and the infant, contributing to the emotional and psychological well-being of both.
However, there are circumstances where a mother may not be able to produce enough breast milk or may be unable to breastfeed due to various reasons like medical conditions, medications, or personal choices. In these situations, infant formula becomes a vital alternative. Formula is scientifically developed to closely mimic the nutritional profile of breast milk, providing essential nutrients that support the infant’s growth and development. While it does not contain the natural antibodies found in breast milk, modern formulas are fortified with vitamins and minerals to ensure the health and well-being of the baby. Please do not worry too much about your child being formula fed.
Problems with Formula-Fed Infants
The use of formula to feed infants has certainly not come without its challenges. Before modern refrigeration and food storage techniques were standardized, the formula-fed infant mortality rate would increase in the summertime due to formula spoilage. There are also cases where parents attempt to stretch the formula by adding additional water. Diluting formula has lead to malnourished infants and sometimes death.
No one would debate that formula is a better means of nutrition for babies when breastfeeding is a viable option.
When Breast Isn’t Best
When the emotional and physical tolls on the mother, and milk producer, are beyond the benefits to the baby breast is no longer best. To rephrase, if the mother can’t make milk, or it drives her into post-partum depression (putting herself and her infant in potential harm’s way), then formula feeding is a safe and viable option.
Breast is not always best, because it’s not always an option.
Fed is Best
Throughout my personal struggles with breastfeeding, I’ve noticed that the tone of the conversation has started to shift. In 2009, when my son was born, breast is best is the only infant-feeding slogan I’d heard uttered. The guilt and shame associated with formula-fed infants were alive and well. I personally felt this guilt and shame as I cried my eyes out in my doctor’s office when we I finally had to come to terms with the fact that my only option was formula feeding.
However, the birth of my daughter has shown me that the tides are starting to turn. While the lactation consultant still did not address my concerns over a lack of milk production, other people involved in my care did. My insurance provided healthy maternity benefits and I spoke with a lactation consultant who stated: “Fed is best.” She encouraged my breastfeeding but stated that if the stress and burden of trying to produce a tiny amount of milk began to take away the joy of my new baby, then there would be nothing wrong with formula feeding my baby. It was the first time I had heard this phrase so I began to look further. Throughout the internet I found articles and resources backing up this new infant-feeding slogan that could help more women feel less guilt.
Best Formula for Breastfed Babies
Picking the best baby formula is a big decision. Most parents will stick with the formula that the hospital provided or recommended by their hospital. In many cases, this going to be some version of Similac or Enfamil. The popular choices at the moment are Similac Pro-Advance or Enfamil Neuro Pro. As long as your baby is gaining weight, isn’t terribly irritable/gassy, and is meeting developmental milestones, you can continue using what they started on. It’s generally recommended to avoid switching your babies formula frequently as each change requires some acclamation from your babies digestive tract, which may be uncomfortable for them.
- EXPERT RECOMMENDED DHA: Enfamil NeuroPro Infant has expert recommended brain building DHA
- HuMO6 IMMUNE BLEND: Enfamil NeuroPro Infant has an exclusive HuMO6 immune blend for immune support
- BRAIN-BUILDING NUTRITION: Get brain building nutrition inspired by breast milk from Enfamil
- ONLY BRAND TO HAVE TRIPLE PREBIOTIC IMMUNE BLEND: Enfamil is the only brand to have both expert-recommended DHA & triple prebiotic immune blend
- Enfamil helps in Brain-building & Immune Support
- PEDIATRICIAN RECOMMENDED: Enfamil infant formula brand recommended by pediatricians
Both of these formulas are advertised as “closest to breast milk.” They are cow’s milk and are a good starting point. If your baby experiences gas, diarrhea or other issues with either of these products, you should discuss options with your child’s primary care provider. For example, if your child has excessive diarrhea and bloating, they may have a milk protein sensitivity and your doctor may recommend a formula that is more broken down such as Similac Alimentium. The cost of this formula is considerably higher. For example, the 19.08 cans of Similac Alimentum is around $40 for a cost of $2.02 per powered ounce. Similac Pro-Advanced is around $36 for a cost of $1.17 per powered ounce. It also goes on sale far less often and can be more difficult to locate in a store. If you think your baby may have a sensitivity, your baby’s pediatrician can perform a hemoccult on a stool sample to confirm. They will then to determine if a formula switch it’s right for your child.
Learn More Infant Feeding Options at the Fed is Best Foundation
I wanted to share a valuable resource for mothers who can’t breastfeed: The Fed Is Best Foundation.
This article isn’t sponsored in any way. I have personally been affected by insufficient breast milk. I want other mothers to know there is no shame in formula feeding their child. If at all possible, breastfeeding is a wonderful option that will provide optimal nutrition for your baby. But if it isn’t, formula feeding is fine.
Download Nurse Bingo Today!
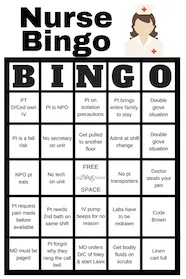
Liven up any shift with a fun game of bingo. See who can fill a row first!
Fill a whole card and lose grip with reality.
Your privacy is protected. We will never spam you.





Oh how I wish I would have had that support! In 1993, the lactation consultant actually threw a fit when I went back to work (in Pediatrics iCU) and she found out I was giving my child formula. We had tried for 6 weeks, and by then my husband and my mother were both insistent we WERE bottle feeding. Opposing opinions sure didn’t help my adjustment to motherhood for sure. My daughter’s pediatrician was supportive, however, because her concern also was “Fed is best “. Poor baby screamed and had horrible diarrhea stools no matter what did when I was breastfeeding. She did keep gaining weight…just didn’t tolerate milk protein in any form. And still doesn’t at 26.